Bharati Sethi, Western University
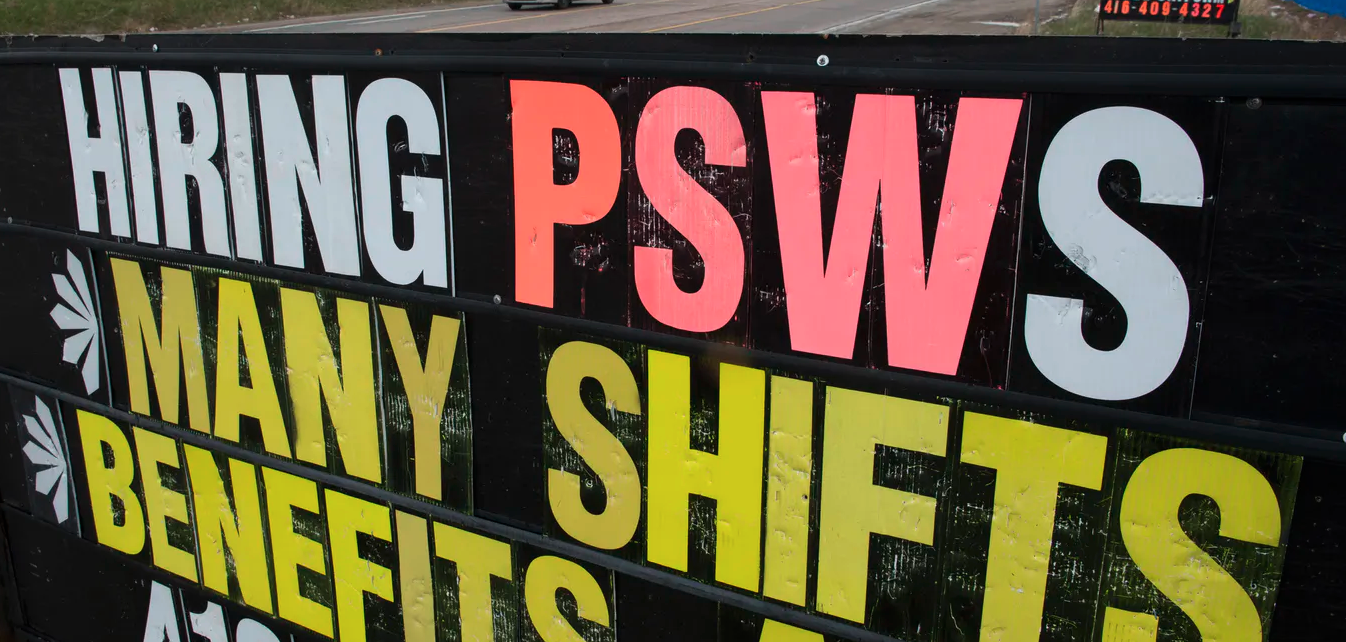
The COVID-19 crisis has highlighted the significant contribution personal support workers (PSWs) make to Canada’s health-care system. As the backbone of much of the daily health work, they assist people with disability, health and age-related needs in diverse health-care sectors and in people’s homes. It seems like every second, someone requires a PSW for their care.
When I was a student, I worked as a home care worker for the Red Cross. I was often the only social contact my clients received for an entire month. My personal and professional experiences as a racialized, immigrant woman fuel my academic research.
For my research, I used a method called photovoice in which participants use cameras to record and reflect upon their lived experiences. I gave immigrant women cameras to record their resettlement experiences in Grand Erie, Ontario.
Through their photographs, the PSWs in the study shared their work experiences.
Stories from PSWs
Black PSWs depicted their experiences of racism and highlighted intersecting issues: race, colour, immigration status and geography.
Ruvashe, a Black refugee, had a supportive relationship with her manager and co-workers, but many of her clients treated her with racism.
She wrote:
“Working as a PSW, the big challenge was being a woman of colour, some of the older people do not have the tolerance for people of a different colour. One of the most interesting incidents that I had was with this old lady, she had a bowel movement, and she was covered in this bowel movement, everywhere — the bed, the walls, her hands, her hair. And I went in, and I said: ‘Hi, I am going to help you clean up,’ and she was like, do not touch me with your Black hands.‘”
Another participant, Rudo (not her real name), shared a similar incident:
“I have to clean my hands. I have to clean my clients. I have to wash them. But they see my Black hands. Some of the clients and also co-workers laugh at me when I wash my hands. They think Black hands are dirty even if I wash them.”
Managers’ responses in these facilities where women were employed varied. One manager brought the issue to the attention of the client’s family who didn’t want Rudo washing her. Others told her not to take the incidents personally as the clients were elderly and “not used to Black people.”
Other PSWs said the retirement home residents often referred to them as “bunch of n- – – – – -” or “the Black girl.”
In a second study on carers in Grand Erie, I worked with with McMaster University researcher Allison Williams. We found similar racialized and gendered narratives of care-giving.
In this second study, Ena, who worked as a registered nurse practitioner in a long-term care facility, said:
“I encountered a lot of racism. And if I did not love what I do, I probably would have given up, because I have a passion for nursing, and I wanted to go further.”
Increasing demand for PSWs
My interviews with managers and employers confirmed the rising demand for health-care workers, especially in the older adult care sector.
Even though immigrant women from racialized populations are a rapidly growing population, they are more likely to be employed in lower paid jobs than Canadian-born and white workers
For example, racialized women make up 13 per cent of the total workforce, but 25 per cent of workers in nursing and residential care facilities and 27 per cent of workers in home health-care services. That is twice the share of the total Ontario work force.
Read more: Inquiry into coronavirus nursing home deaths needs to include discussion of workers and race
The costs of front-line work
PSW work is physically, mentally and emotionally demanding and characterized by precarious employment. Many of the workers hold multiple jobs to make ends meet, as I did to pay my university tuition.
Experiencing racism while managing a demanding, precarious, and low-paying job can be detrimental to employee’s health and psychosocial well-being. Race is a social determinant of health, but it also can have enormous socioeconomic costs.
PSWs and other health-care workers have been at the front lines of the COVID-19 pandemic, working selflessly to care for the ill and vulnerable. They experience anxiety, stress, occupational burnout, fatigue, guilt and fear. A few even died
Urgent need for policy
Employers and supervisors in health-care facilities must commit to a Call for Action to address systemic racism through anti-racist policies and make their workplaces carer-friendly for all their carer employees.
The Employment Outlook (2019-2021) noted that along with those who leave school, a significant number of new immigrants belong to the PSW occupational grouping. Considering that many of those workers will inhabit Black, Brown, immigrant and/or refugee bodies, one of them will be taking care of each of us or our family members at some time in our life.
Read more: Inquiry into coronavirus nursing home deaths needs to include discussion of workers and race
PSW work has low requirements and allows immigrants to quickly find employment, enabling them to gain Canadian experience, one of the most significant barriers for immigrants.

Women in these two studies volunteered and worked in jobs considered low-skilled to gain Canadian work experience in hopes of finding skilled employment with better wages and working conditions.
Evidence from my studies and other research suggests that immigrant care workers are loyal to their employers and show care and respect for their clients, despite enduring harsh conditions.
There is an urgency for policy-makers to prioritize PSWs’ working conditions and wages if they hope to sustain a robust health-care system. Sadly, it has taken COVID-19 to highlight the significant contribution to our collective well-being made by PSWs and other health-care workers. However, the voices of racialized PSWs remain at the margins of care discourse. They are indeed the unsung heroes.
A common hope expressed by study participants was that increased diversity outside large urban centres would help drive new policies and programs to address racism. But diversity without meaningful inclusion is not beneficial to the workers, their employers or society at large.
Bharati Sethi, Associate Professor, Western University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
If you are interested in contributing to Voices from the Margins of a Crisis, please email Tanya Benjamin at tbenjam4@uwo.ca and Eaman Fahmy efahmy@pillarnonprofit.ca
Listen to an interview with Dr. Bharati Sethi on 980 CKNW (aired on September 5, 2020)